GMO bacteria to target tumours
PhD candidate Jella van de Laak on how a genetically modified bacterium fights solid cancer tumours at their oxygen-deprived core.
What exactly is cancer? “A normal cell with bad programming which proliferates continuously,” explains Jella van de Laak, PhD candidate at GROW, the Research Institute for Oncology and Reproduction at FHML. “Normally the body’s immune system detects this bad programming and kills the cells but with cancer, for several reasons, that’s not the case.”
How can we treat solid tumours?
One possible treatment is immunotherapy, an approach centred around mobilising the body’s natural defences. “Your immune system is really complex and beautiful; it’s like an army that detects anything harmful, from pathogens like bacteria or viruses to any rogue cells in the body.” Immunotherapy refers to several ways of using this system to fight cancer; it is already used in clinical settings. “The problem is that it’s not very localised; the inflammatory response that is meant to kill the tumour affects the whole body, which results in side effects.”
Together with Jan Theys and Ludwig Dubois, her colleagues at the department of Precision Medicine, Van de Laak has developed an approach in which they use genetically modified bacteria to deliver immunotherapy directly and exclusively to the tumour. Because cancer cells proliferate fast, the tumour grows progressively denser until blood can no longer enter due to vascular disruption. The tumour becomes hypoxic, i.e. deprived of oxygen. “This makes the tumour very difficult to treat because chemotherapy is delivered through the blood and radiotherapy requires oxygen. Also, there are barely any immune cells in such hypoxic tumours because the environment becomes slightly acidic.”
Genetically modified bacteria to the rescue
Van de Laak’s tiny knight in shining armour is Clostridium sporogenes, a bacterium that grows in the absence of oxygen. “The necrotic areas of tumours seem to be the perfect niche for this bacterium.” She intravenously injects the endospores, a stripped-down, dormant form to which the bacterium can reduce itself. Only once these endospores reach and leak into the necrotic parts of the tumour, do they find an environment favourable enough to germinate and proliferate inside the tumour.
However, this only causes a mild immune response, possibly because Clostridium is familiar to the immune system from being present in our gut. “That’s why we’ve genetically modified the bacterium to deliver immunotherapy and kick-start the body’s immune response from inside the tumour.” The underlying concept has a long history. “To my knowledge, we’re the only ones in the Netherlands doing this specific type of research; the research area is still quite small. However, bacterial-based anti-cancer therapy started already in the 1800s, but back then the immune system wasn’t well enough understood.” Since they are easy to genetically modify, Van de Laak thinks bacteria have tremendous potential in the fight against cancer.
"After 48 hours, there’s little left of the tumour."
Eenie meenie spheroidic tumour
After stably integrating the desired gene in the bacterium’s chromosomes, the concept needed to be validated in vitro. Normally, this would involve growing cancer cells in a little jar. Hypoxic and necrotic tumour areas, however, won’t develop in the presence of oxygen. Therefore, Van de Laak developed a spheroidic 3D cell model, which she charmingly and, one assumes, unscientifically, refers to as an “eenie meenie tumour.”
The spheroids grow and mimic hypoxia and necrosis as hoped. Van de Laak describes the results as very promising. “In vitro, the spores of the genetically modified bacteria strain diffuse into the mini tumour, colonise the necrotic spheroids and produce immunotherapeutic agents which have a positive effect on the immune cells."
A promising way towards beating cancer
The resulting paper is to be submitted soon. Van de Laak and her colleagues have already moved on to in vivo studies, the logical next step to progress towards a clinical application. The effects of Clostridium colonising the tumour can be observed immediately. “After 48 hours, there’s little left of the tumour. If you cut it open, it’s like a burrata,” she explains merrily, and just after lunch. She describes animal research as emotionally taxing. “I feel responsible for their wellbeing, but I also know that, currently, there’s no other way to study this because mimicking the full immune system isn’t possible in vitro – it’s way too complex.”
While the science looks promising, the politics might still be an impediment. “People are still reluctant when it comes to both bacteria and GMOs,” reflects Van de Laak, “and I understand that, but we shouldn’t miss out on possible therapies because of that. Especially because Clostridium allows us to insert any gene we like. Beyond tumour-specific delivery, this could be used for individually tailored therapies. We must think outside the box – I think radiotherapy and chemo alone won’t cut it.”
In love with the immune system
Oncology has been Van de Laak’s dream since high school. “Back then, I wanted to be a medical doctor, but I wasn’t smart enough,” she laughs, referring to her HAVO diploma, the second tier of Dutch secondary education. After a brief stint studying theatre, she pursued a bachelor’s degree at Zuyd University of Applied Sciences, then a master’s degree in Biomedical Sciences at UM. “I fell in love with the immune system, the complexity of it, the collaboration and communication between different types of cells and pathways. It’s fascinating and still very new, so there’s so much to investigate. Obviously, it’s relevant because it has the power to cure diseases but also cause them.”
Finishing her master’s programme and working as a lab technician at MUMC+, it was clear to Van de Laak that she wanted to work for GROW at the intersection of oncology and immunology. “I emailed my contact there and told them I wanted to work in that field, no matter the position. That’s how I learned about the PhD position on Clostridium. It’s been a steep learning curve but it’s amazing to have all this freedom along with the guidance of experienced researchers.” She is enjoying the environment and colleagues at GROW and hopes to continue there. “But basically, my attitude has stayed the same, I want to contribute to this field, no matter how.”
Text: Florian Raith
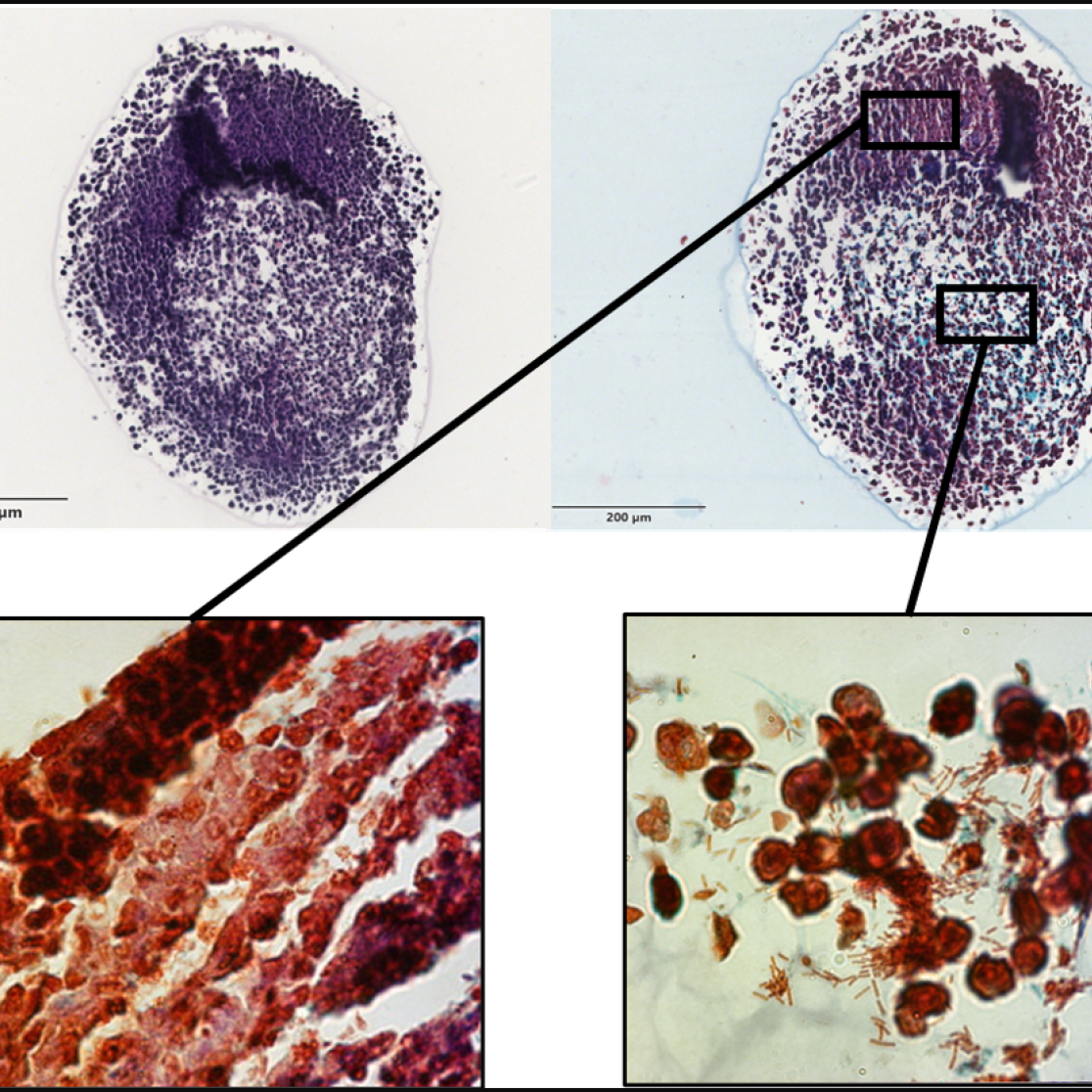
Top: H&E- and Gram-stained spheroid; 4x magnification
Bottom: Clostridium colonising necrotic tumour area; 60x magnification
Also read
-
Fresh air
Newly appointed professor Judith Sluimer (CARIM) talks about oxygen in heart functioning and the 'fresh air' the academic world needs.
-
GROW research: all-in-one test for genetic defects in embryos🧪
Researchers at Maastricht UMC+ and GROW have developed a technique that can analyse the entire genome in a single test, allowing for faster determination of embryos suitable for successful pregnancy.
-
Prestigious European grant for three UM researchers
Three researchers from Maastricht University (UM) will receive a prestigious ERC Starting Grant from the European Research Council. They will receive €1.5 million each. Their funding is part of the EU Horizon Europe programme.