Home surgical models
Ischemia-reperfusion damage in digestive tract and liver
Ischemia-reperfusion injury is a pathophysiological phenomenon in a variety of diseases. To find new targets for therapy and characterize pathophysiological events during ischemia, innovative human experimental models were developed at the department of Surgery.
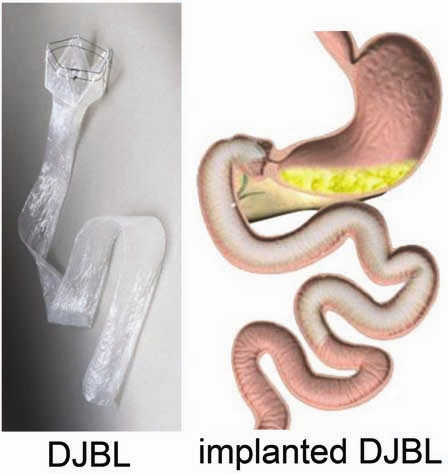
A variable length of healthy jejunum is usually resected in patients undergoing pylorus preserving pancreatico-duodenectomy, of which a small part is used for study purposes. This intestinal segment, provided with a central mesenteric arteriole and venule, (Figure 1A, white arrows indicate mesenteric vessels) is isolated by transection at both ends with a linear cutting stapler (Figure 1B). Thereafter, ischemia is induced for up to 60 min by placing two vascular clamps (Figure 1C, asterisk) across the mesentery. This leads to discoloration of the jejunal wall (Figure 1D, white arrow). Meanwhile, surgery proceeds as planned. Removal of the clamps initiates reperfusion as confirmed by regaining of normal color and restoration of gut motility. Tissue is sampled at different time points throughout the procedure. Blood is sampled at the same time points by direct puncture of the venule draining the isolated jejunal segment. In this manner, we are able to monitor the temporal behavior of biological processes over a period of progressive injury and subsequent initiation of repair. This can be seen from the histological stainings in (Figure 1E) from left to right depicting control tissue, tissue harvested directly after ischemia, and after 30 and 120 minutes of reperfusion. In addition, the blood samples are used for biomarker discovery and to validate our newly developed assays to evaluate intestinal function and integrity. Of note, the procedure only minimally prolongs surgery, making this a harmless, minimally invasive procedure for patients. This model has led to novel insights into human intestinal pathogenesis with respect to barrier disruption, onset of inflammation, cell death, and loss of antimicrobial defense. A similar human model was developed for colon.
Another surgical procedure, the so-called Pringle maneuver during which intermittent hepatic inflow is occluded to minimize blood loss during liver surgery, enables the study of ischemia-reperfusion induced hepatocellular damage.
Information: Dr. Steven Olde Damink, Department of Surgery
Obesity treatment
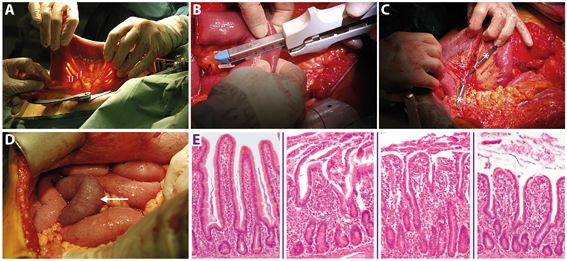
Obesity, type 2 diabetes mellitus, and nonalcoholic fatty liver disease form a worldwide epidemic with great morbidity and mortality. These diseases are treated and studied using innovative surgical techniques. For example, we are pioneering a novel minimally invasive alternative for conventional bariatric surgery, the so-called ‘Endobarrier duodenaljejunal bypass liner’ (DJBL). This device constitutes a 60 cm open teflon sleeve, which is placed endoscopically in the proximal small intestine, effectively excluding this part of the gut from exposure to food. We and others have shown that it rapidly improves type 2 diabetes before significant weight loss occurs. Our most recent data indicate that changes in the postprandial release of the gut hormones GLP-1, GIP, glucagon, and PYY play a major role in the rapid amelioration of type 2 diabetes. Ongoing studies are directed at the DJBL-induced changes in gut microbiota composition, satiety hormones, and plasma parameters of nonalcoholic fatty liver disease.
Information: Dr. Steven Olde Damink, Department of Surgery