Ozempic – obesity solved?
Obesity is one of the great public health problems we face. New drugs such as Ozempic offer possibilities but also raise moral, economic and health questions. Why is ‘just lose some weight’ naïve and unempirical? Why might covering Ozempic be cheaper for health insurers? We brought together experts Anne Roefs, Gijs Goossens and Mickaël Hiligsmann to talk about obesity and its new miracle cure.
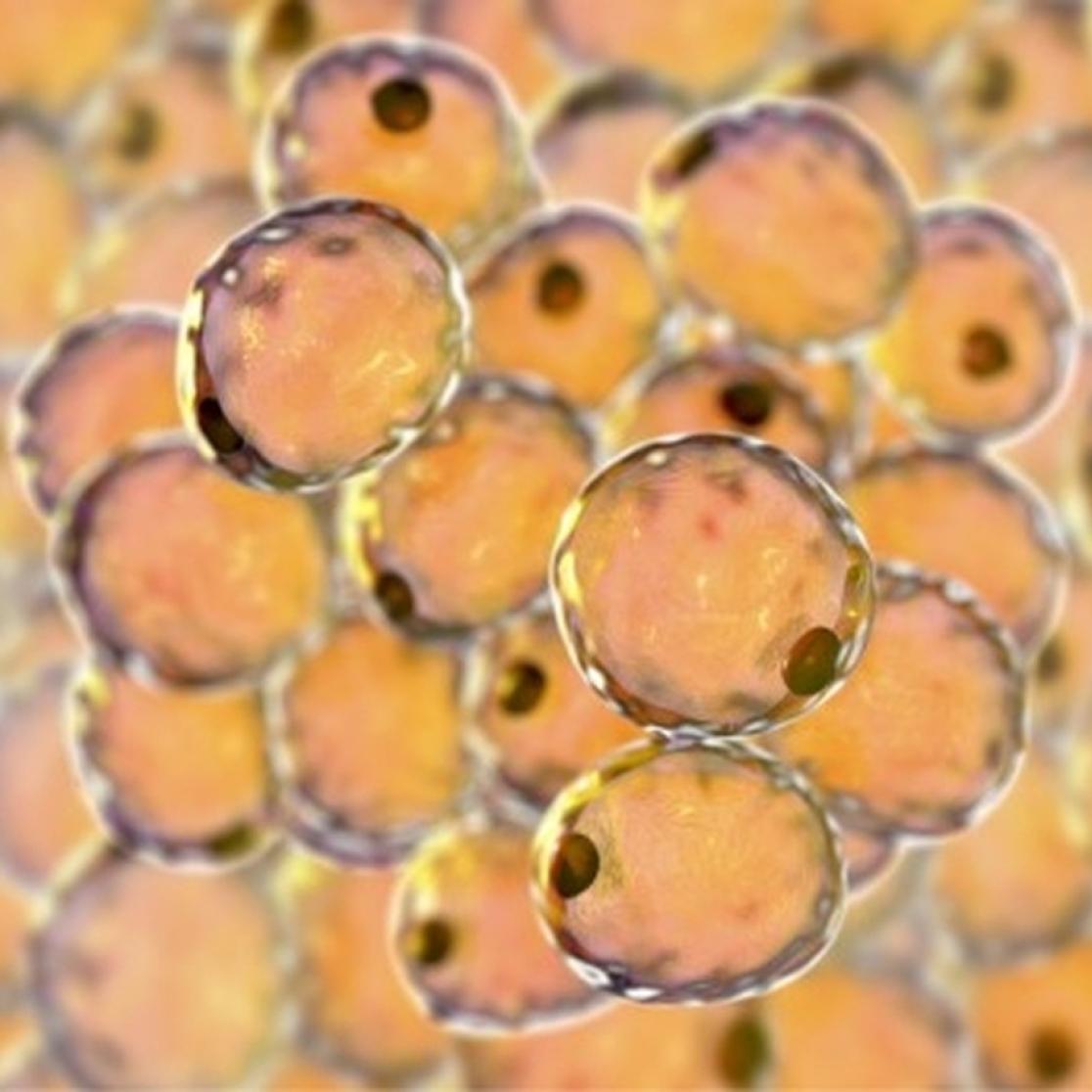
It is possibly the most consequential and lucrative innovation to come out of Denmark since Lego and coastal raids in longboats: Ozempic. Often touted as a miracle drug, it was developed by the Bagsværd-based multinational Novo Nordisk as a treatment for diabetes; its active ingredient semaglutide, like insulin, decreases blood sugar. A side effect that quickly took centre stage is that this reduces appetite, or better increases and prolongs satiety. Patients feel full for longer; as a result, they eat less and lose body weight.
Losing excess weight does not only improve quality of life. Besides inviting judgement, obesity has serious medical ramifications. Gijs Goossens, Professor of Cardiometabolic Physiology of Obesity at the Institute of Nutrition and Translational Research in Metabolism (NUTRIM), explains that the consequences of obesity are very serious. “Obesity acts as a gateway to many complications and chronic diseases, including kidney, liver, respiratory and cardiovascular diseases, type 2 diabetes, arthritis, cancer as well as dementia”. It is also associated with mental disorders such as depression.
It is important that people realise that obesity is a complex chronic disease.
Professor Gijs GoossensMore complex than akrasia
In principle, weight loss is as simple as consuming fewer calories than one burns. A common moral syllogism is that eating less requires discipline, therefore relying on drugs is somehow cheating. Goossens is quick to push back on that intuition. “Of course, a healthy lifestyle is the cornerstone in the prevention of obesity and related complications. It helps reduce high blood pressure and high levels of cholesterol and blood sugar. Yet, we often need to treat these symptoms with medication to prevent further complications. Few people have a problem with that – but using obesity management medication triggers a different response.”
Goossens also takes issue with the simplistic idea of weight loss and maintenance as a matter of personal virtue. “Yes, in many but not all cases it’s about eating too much but it’s important to understand that obesity is not a lifestyle choice. Research shows that people may gain weight for a variety of reasons such as genetics, chronic stress, an unhealthy diet, physical inactivity, sleep impairments, or side effects of common medications such as anti-depressants, anti-psychotics and long-term use of some anti-inflammatory drugs. It is important that people realise that obesity is a complex chronic disease.”
Eating less vs being healthy
The timeless wisdom ‘just go to the gym’ is misguided as well. While exercising is great for cardiovascular health and long-term health outcomes in general, it does little to contribute to weight loss beyond “building muscles through resistance exercise training. That then causes you to burn more calories – also while resting.” Goossens explains that obesity is the result of a complex interaction between biological, psychological, socio-economic and environmental factors. “You needa holistic approach: On the one hand, you have prevention. The government is responsible for creating a healthy environment to facilitate a healthy lifestyle. At the same time, we must provide better care for those already living with obesity.”
Anne Roefs, Professor of Psychology and Neuroscience of Abnormal Eating at FPN, agrees – and is consequently very sceptical about treating the symptoms at the expense of tackling these underlying reasons. “Because Ozempic acts on satiety, you lose weight by eating less – and that has health benefits, sure – but you’re not necessarily eating any healthier. If, due to taking Ozempic, I eat 4 croissants instead of 6, I’ll lose weight, but I still have a terrible diet lacking in micronutrients and it’ll be impossible to keep the weight off without the medication.”
The unhealthy half-truth of individual responsibility
This is not to say that Roefs rejects pharmaceutical treatment in all cases; but she sees a real problem in the way we frame this and other public health issues: “We are taking a societal problem and focusing on the individual. As in so many other cases, we are seduced by a quick technological fix to a complex systemic problem.” Roefs sees an over-reliance on drugs as shortsighted since it takes away incentives for governments to regulate the actual causes of obesity and for individuals to cultivate a healthier lifestyle.
Both of those would require increasing the friction between people and unhealthy, hyper-palatable food. The obvious way forward is doing to high-fat, high-sugar food what we have done to cigarettes. Yet, many people are understandably allergic to the state telling them how to live. “But industry is constantly telling you how to live, what to buy, what to eat. It’s so much more than advertising; it’s our built environment from cities designed exclusively for car use to supermarkets offering 80% unhealthy food. How free are you really? We live in a world where living a healthy life requires a lot of effort.”
Last resort or shortcut?
Roefs is happy enough to concede that these drugs are an effective intervention but thinks that it’s a bad idea for most people to take them. “I see a danger here. It’s naïve to think that people will only use it as a last resort.” On the back of a wave of publicity from influencers and celebrities using Ozempic for aesthetic ends, survey data suggests that 1 in 8 adults in the United States has used Ozempic-like drugs at some point, and half of those – around 15 million people – are currently using it. Some might say this couldn’t happen in the Netherlands where you need a prescription from your GP, but Roefs tried to order Wegovy, developed by the same company and with the same active ingredient, and managed to do so in less than 5 minutes.
“I filled in an online questionnaire faking the answers and voila, for a bit more than €500 I would have been able to order a month’s supply.” This also means that there is competition for this limited resource between those for whom it is a potentially lifesaving treatment and those who are willing to invest their disposable income in visible abs or a thigh gap. Even if we discard that consideration and view Ozempic purely as a medicine, there remains the question of who covers the cost.

Gijs Goossens is Professor of Cardiometabolic Physiology of Obesity at the Institute of Nutrition and Translational Research in Metabolism (NUTRIM), an institute withing FHML which works closely with the Maastricht University Medical Centre+. He is Chair of the Scientific Advisory Board of the European Association for the Study of Obesity.
A few years ago, we conducted a cross sectional survey that revealed the total costs of obesity to be around €10,000 per year per person
Associate Professor Mickaël HiligsmannExpensive weight loss still cheaper than status quo?
If we frame obesity as a personal moral failing, then it seems odd to ask health insurances to cover medications that aid weight loss. Leaving aside for a moment that this view is deeply flawed, there is also an amoral case to be made in favour of drugs as expensive as Ozempic: “A few years ago, we conducted a cross sectional survey that revealed the total costs of obesity to be around €10,000 per year per person,” explains Mickaël Hiligsmann, associate professor at UM’s Care and Public Health Research Institute (CAPHRI). “Of this sum, less than half was health care costs; the rest was ‘societal costs’, that is to say productivity loss because the person or their informal carers skip work or leisure activities.”
Hiligsmann explains how the Netherlands National Health Care Institute (Zorginstituut) earlier this year rejected to reimburse Wegovy. They concluded that its efficacy is beyond doubt but that long-term effects are as yet unclear and that the costs were prohibitive. “Seven million people in the Netherlands are seriously overweight and have associated health complaints; it would cost €1.3 billion per year to treat them with Wegovy.” A lot of money but still only half of what Chelsea have spent on players in the last ten years. (This to put the number in perspective, not to suggest the London football club fund weight loss in the Netherlands instead…)
At the same time Hiligsmann points out that there is always a trade-off. “Of course, a country’s resources are limited, and tough choices have to be made. It is clear that the burden, not only economically but also in terms of quality of life, due to obesity is rising, so it’s important to prevent and treat in a cost-effective way. For that, we need to compare interventions such as obesity management medication or bariatric surgery. It could well be the case that, as the price goes down and the availability increases, Ozempic will be reimbursed by health insurers.”
The value of pharmaceutical weight loss interventions becomes more obvious when we clearly distinguish terms. The BMI (Body Mass Index) is calculated as kilogrammes per height in metres squared. As Goossens himself has pointed out in a recent article suggesting a different framework for obesity diagnostics, BMI is not very accurate for individuals. Following its formula, a rugby player could be ‘obese’ despite having 10% body fat. However, it requires very little data to calculate and holds up well across populations – also due to the relative scarcity of rugby players. Overweight starts at a BMI of 25 – think a man of 1.8m and 81kg – whereas obesity starts at a BMI of 30 – the same man weighing 98kg.

Mickaël Hiligsmann is Associate Professor in Health Economics and Health Technology Assessment at the Care and Public Health Research Institute (CAPHRI), FHML, and is Editor-in-Chief of Expert Review of Pharmacoeconomics & Outcomes Research.
Very preliminary results suggest that the best results are obtained by those who manage to change their habits in daily life
Professor Anne RoefsMerits and limits of lifestyle interventions
Goossens explains that lifestyle interventions – diet and exercise – should always be the first step but is also quick to point out the limitations of self-discipline and good advice: “There are people with a BMI of 40 or higher who need to lose a substantial amount of body weight to prevent complications. The longer you remain outside of the danger zone, the better for your long-term health outcomes. Obesity management medication such as semaglutide is more effective in lowering chronic disease risk and improving quality of life compared with lifestyle interventions in certain patients with severe obesity.”
Roefs, however, wonders whether the results of Wegovy – 10% weight loss after 4 years, almost all of which occurs during the first couple of months – wouldn’t be possible gradually and sustainably through a healthier lifestyle. “These lifestyle interventions [ideally consisting of group therapy and cognitive behavioural therapy along with a diet and exercise regime] aren’t about hectoring people. Most people know in theory what a healthy lifestyle is and don’t need more health information. During an intervention, you try to fathom why they find it so hard to eat healthily and exercise sufficiently. Then you implement strategies on how to cope and make healthy lifestyle changes.”
Roefs stresses that a shift in mindset is necessary to cultivate a healthy lifestyle over time. “It’s not lack of will power but our environment that promotes an unhealthy lifestyle and deeply entrenched unhealthy habits. Life is not always easy and not everyone faces the same challenges.” Roefs is currently leading a project studying what psychological, behavioural, environmental, personal and biological characteristics determine how effective an intensive lifestyle intervention is for individuals, also in the long run.
“Very preliminary results suggest that the best results are obtained by those who manage to change their habits in daily life,” explains Roefs, who finds the idea of temporary diets self-defeating. “You can never go back to the eating patterns that made you obese in the first place. A healthier lifestyle over time is more sustainable – and a better example for your children: rather than go for a quick fix, you are actively taking care of yourself.” She is quick to acknowledge just how hard it is to change habits and that it will be a gradual and lifelong process, during which proper support is needed.

Anne Roefs is Professor of Psychology and Neuroscience of Abnormal Eating at the Faculty of Psychology and Neuroscience’s (FPN), where she chairs the Eating Disorders and Obesity section.
Roefs thinks trying to consume our way out of the situation is problematic. “We now have a situation where the food industry through marketing and ultra palatable calorie-dense, nutrient-poor food is making huge profits and causing a lot of damage. Instead of regulating them, now the pharmaceutical industry is making huge profits. In response, Nestlé for example has launched a food brand aimed at GLP-1 users, so those on weight loss medication.” The profit motive matters because these pharmaceuticals are not a cure but a chronic treatment: patients have to continue taking them – or regain the weight.
Holistic changes rather than band aids
Metabolism expert Goossens agrees that, once the bodyfat percentage is back in the green, there’s likely no happy-ever-after. “Studies have shown that, on average, more than half of the initial weight loss is regained after two years and more than 75% within 5 years. Our body fights weight loss by increasing hunger and reducing energy expenditure.” While most of the weight lost is fat, around 30% is muscle mass, which partially explains this reduction. “Actually, the decrease in energy expenditure is even lower than we would expect based on changes in body composition. This phenomenon is called ‘metabolic adaptation’, but the underlying mechanisms are not yet fully understood.”
This means that once a person with obesity has reached a healthy weight, they can consume fewer calories to remain weight stable than someone with the exact same body composition who hasn’t been obese – and they’ll feel hungrier. The answer would be Ozempic in the long run. Goossens would again point to the fact that we do this for other diseases too but concedes that it’s problematic that we live in a world where this should be necessary and common. People not getting obese in the first place would be preferable for a litany of reasons. While Goossens and Roefs do not fully agree on whether weight loss drugs are a crucial intervention or a distraction from the actual changes that need to happen, they very much converge on those necessary changes.

For Dutch-speakers only:
Vind jij het ook belangrijk dat we de obesitaspandemie beter begrijpen, en wil je bijdragen aan effectievere en persoonlijkere behandelingen voor overgewicht? Meld je dan nu aan voor dit onderzoek! Vooral mannen (van elke gewichtscategorie) en vrouwen met een gezond gewicht of met overgewicht (BMI 25-30) zijn welkom.
These include a society where the healthy choice is affordable, easy, and attractive, where all children learn good habits early, independent of their socioeconomic background, where chronic stress, precariousness and loneliness are exceptions, not the norm. Both also agree that ‘health at every size’ is a dangerous myth but are quick to stress that the stigma around obesity is counterproductive as it does more to keep people away from healthy behaviours. Roefs adds that, while lifestyle changes need to be permanent, they don’t have to be absolute. “Living and eating healthily around 80% or 90% of the time is good enough.” Still space for the occasional croissant then.
Text: Florian Raith
Also read
-
SHE Educates on demand
Within SHE Educates, we are introducing our On Demand courses - courses that can be given anytime during the year, based on your availability and schedule. Below, you can find more information about which courses we offer on demand, as well as and other related information.

-
Introducing the new MHPE Management Team
As of September 1st, 2025, the new MHPE Management team has been installed. Led by Renée Stalmeijer, co-coordinated by Boukje Compen, and further strengthened by Jimmy Frèrejean, the new team is looking forward to building on the strong foundation laid during the curriculum revision.
-
Maastricht University School of Business and Economics honoured at 20th anniversary of Prix FIR-PRI
On 1 October 2025, during the 20th anniversary celebration of the FIR-PRI “Finance & Sustainable Development” Prize in Paris, Maastricht University School of Business and Economics (SBE) received a special recognition for being one of the most awarded institutions in the history of the prize.
Hosted...
